Please note that this is my personal medical story. There are details of medical procedures. I am not a medical doctor.
I had a couple of weeks' wait in between hearing from the breast surgeon that I would most likely need chemotherapy and radiation and the appointments with the oncologists. I was surprised to learn that the oncologists specialise in either medical oncology (chemotherapy and hormone therapy) or radiation oncology, not both, so I had to see two different oncologists on different days.
In a nutshell, chemotherapy targets the whole body in case there are any cancer cells travelling around and radiotherapy targets a specific area, the breast in my case, to kill any cancer cells that may have been left behind after the surgery. Some breast tissue is always left behind as it looks the same as the underlying tissue, so it's impossible for the surgeon to remove it all. Sometimes chemo and radiation are used before surgery to shrink the tumours. It just depends on the individual case and what the specialists think is best. The purpose of both treatments is preventing the cancer coming back.
 |
| These books from the Cancer Council were a very good source of information |
After I picked myself up from the shock of needing more treatment, I did what I always do and started reading about the treatments so I knew what to expect. My partner and I are both former research scientists, so we got technical and read some research papers in addition to the reputable breast cancer websites (eg
BCNA,
breastcancer.org). I kept asking my partner questions to get everything straight in my head. Luckily he has endless patience! I wrote down questions (lots of questions!) to ask at the appointments. I also decided I should get myself fit again so I was ready to face whatever was coming next. I got up early and went for walks, trying to go a bit further or faster each day. I also had some fun days out with the family.
Medical Oncology - Chemotherapy
On the day of the chemo appointment, my partner and I had to arrive 45 minutes early so we could do a Rapid Antigen Test (RAT). Western Australia is on Level 2 restrictions and nobody can enter the oncology ward if they are Covid positive. This is because chemotherapy lowers immunity making patients more susceptible to infection. The rules also stated that only essential carers were allowed in with patients, no other support people. We were questioned on our way in and I said (as confidently as I could muster) that I'd been told to bring someone. This seemed to work and we were both allowed in. I really think that a support person is essential in this kind of appointment where lots of information is given, so they can take notes and ask questions.
The oncologist was lovely and spent a long time making sure I understood everything. I was very grateful not to feel rushed. There was a lot to take in. I will try to explain it as clearly as possible.
Initially she talked about the benefits versus the risks of chemotherapy in my particular case. She used an online tool by the NHS called
Predict. The website asks for information about the patient, such as age and menopausal status and about their cancer, such as oestrogen status, HER2 status, tumour size etc. From there, the website makes a prediction based on the percentage of people with similar characteristics and similar cancer who are still alive after 5, 10 or 15 years with surgery only, surgery plus hormone therapy or surgery plus hormone therapy plus chemotherapy.
PLEASE NOTE that this does not work for all types of breast cancer and the results should be discussed with your oncologist as the benefits and risks of chemotherapy need to be assessed by an expert.
 |
| Part of the NHS Predict online tool showing my data |
In my case, the results showed that 10 years after surgery 76% of people with similar characteristics to me, who had surgery only, were still alive (in people without breast cancer 95% would still be alive after 10 years as 5% of people in this group die from other causes). If patients had hormone therapy in addition to surgery, the 10 year survival rate increased to 82% (a 6% increase) and if chemotherapy was added in as well, the survival rate increased a further 3% to 85%.
This means that hormone therapy provides a large benefit with a low risk. Hormone therapy has less side effects and a lower risk than chemotherapy. Hormone therapy is a definite for me. Adding in chemotherapy adds 3% to the chance of surviving to 10 years for people in my cohort. So the decision needed to be made whether the risks and side effects of chemotherapy are worth taking for an additional 3% chance of survival....
....how does anyone make a decision like that? How do I know if I'm in the 3% who will benefit from chemotherapy? I don't want chemo, but I'll have it if it means I won't be dead in 10 years.
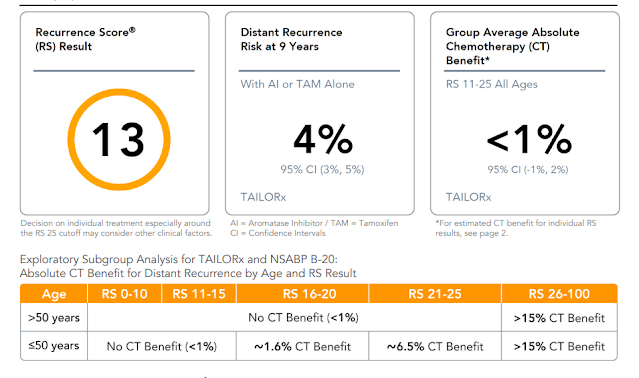
Fortunately there is another test that can predict the benefit of chemotherapy much more accurately. However, it can only be used in breast cancer patients who have early, invasive ductal or lobular cancer which is oestrogen receptor (ER) positive, HER2 negative and with a maximum of three lymph nodes positive. It also assumes the patient is going to have hormone therapy. I have early stage, invasive lobular, ER+ve, HER2-ve breast cancer with no lymph node involvement. I'm a candidate for the test!
The test is called the Onchotype DX and is done in a lab in the US. It is available for breast, prostate and colon cancer. This explanation is from the
Exact Sciences website:
"Studies have shown that chemotherapy does not reduce recurrence risk in all breast cancer patients by the same amount. In fact, only a minority of patients with early-stage, node-negative breast cancer substantially benefits from chemotherapy whereas the vast majority of patients doesn’t benefit from it and can be spared this treatment and its related toxicities. Without the right genomic test, doctors can only estimate how likely a patient’s cancer is to return. By adding the information from a genomic test that is proven to predict chemotherapy benefit, your doctor can more precisely assess how likely a tumour is to respond to a treatment like chemotherapy."
The lab uses samples from the tumour (or biopsy) that has been removed, so there are no further tests for the patient. The genes are analysed using genomic testing to provide information about the biology of the cancer. The result is given as a score, which enables the oncologist to tailor treatment and decide whether chemo is necessary. This is different to genetic testing, which can give information about a patient's likelihood of getting certain cancers. In summary, genomic testing determines the benefits of chemo and type of treatment necessary, genetic testing determines the risk of getting cancer.
The Onchotype DX test costs AU$5000 for Australians and is not covered by Medicare. I believe that groups are lobbying the government to have it covered by Medicare, which would make sense given the enormous cost of providing chemotherapy. The test has been done on over a million people so far and causes treatment decisions to be changed in around 25% of people. This means that one quarter of people who have been recommended to have chemo, or not have chemo have the decision reversed after getting the test results.

Next we talked about chemotherapy and what would be involved in my case. There are two possible regimes for me, both with similar side effects. One is called TC (docetaxel and cyclophosphamide), which would be four treatments, one every three weeks. The other is AC-T (doxorubicin hydrochloride [Adriamycin] and cyclophosphamide, followed by treatment with paclitaxel [Taxol]) which would be eight treatments, one every two weeks. The side effects include hair loss, nausea and vomiting, constipation or diarrhoea, nail changes, mouth ulcers, fatigue and altered taste. The risks include an increased chance of infection which would require going to the emergency room for an antibiotic infusion with any fever over 38C, nerve damage causing numbness and tingling, menopause, heart problems and a low 0.05% risk of cancer caused by the chemotherapy.
So, after all this discussion and getting answers to my long list of questions, I needed to make a decision. I could have gone away to think about it if I wanted. The oncologist said it was up to me what treatment I had. She said some people want to 'throw everything' at the cancer and have the chemo and some choose not to go ahead, even if it's recommended. I wanted to know whether chemo was recommended for me. The oncologist said that I'm borderline for needing chemo, but if she had to make a decision she would not recommend me having it. She said I was an ideal candidate for the Onchotype DX test. For me, that was the decision made. I would go ahead with the Onchotype DX as that should tell me with good accuracy whether I am in the small group that would benefit from chemo. If I am in that group, I'll have the chemo. If not, I can carry on with my life without worrying that I should have had it to stop the cancer returning. We decided that I would wait the four weeks for the test results before starting on hormone therapy.
The following day I had my appointment to see whether I would need radiation treatment. I had decided that, after the encouraging news about hopefully not needing chemo, I would be sure to need radiotherapy.
I saw the registrar first. She took some information, had a look at my new breast and explained radiation treatment in quite a lot of detail. The treatment would target the chest wall and reconstructed breast in a square formation in order to kill any cancer cells that may remain after surgery. I would need a CT scan first so the oncologist could plan where exactly she needed to direct the radiation. I would then have three tiny tattoos placed on my chest, each about the size of a small mole, which would be used to line up the radiation machine perfectly each time. The treatment sessions would last around 30 minutes every weekday for five weeks (this varies by patient) and could be done at a time that suited me. They would involve lying on a bed with my arm raised while the machine delivered radiation exactly where needed.
The radiation is the same as is used in x-rays, so treatment doesn't hurt and the patient does not become radioactive! There is no hair loss, but by about the third week, some skin irritation is likely in the treated area. Other side effects may include fatigue, tenderness, skin pigmentation and irritation/scarring of the lung and heart (since mine would be on the left side). The lung and heart effects are usually short-term, but scarring can remain that would show up on CT scans in the future. Radiation treatment is not like chemo and doesn't have a major effect on day-to-day life. Treatment would start straight away, or after chemo, if I need that, and the hormone therapy would start after the radiation treatment had finished. The results of the Onchotype DX test cannot predict whether a patient would benefit from radiation treatment.
I then saw the radiation oncologist. She was brilliant and explained everything very clearly. She said that radiation is routinely recommended if the tumour size is larger than 5cm. My largest tumour was 5.8cm. However, since my lymph nodes were cancer-free and and the margins were clear (the margin is the cancer-free layer of tissue around the tumour that is removed during surgery, its thickness can vary but is ideally about 1cm), she said I was a bit of a 'grey area' for needing radiotherapy. We had some more discussion and then she said that in her opinion, I would not benefit from radiotherapy, but that hormone therapy was 'non-negotiable'. She also recommended that I consider having genetic testing, given that I have had breast cancer and have a strong family history of bowel and pancreatic cancer. There is a likelihood that these three cancers are linked. Genetic testing would indicate whether I was at increased risk of any these cancers and, if so, I could take preventative action, for example having my other breast removed, increased bowel cancer screening etc.
I can hardly describe how I felt as I left the appointment. Did she really just say I didn't need radiation!? In two days, I'd gone from thinking I needed chemo and radiation and now I probably don't need either. I felt like I'd dodged two major bullets. I was elated. Maybe I should buy a lottery ticket!!
In other news
I am continuing to heal well. I am walking every day and have got back to the pace I was doing before surgery. My tummy skin is not quite as tight as it was, but there is still some swelling, tightness and hardness. My new breast is getting softer and the swelling looks like it’s gone down completely and it is looking more like the natural breast. I am really pleased with the outcome so far. I'm not in any pain, just occasional discomfort in certain positions or turning over in bed.
Last week I had a day at the Crown hotel pool as we had some vouchers (look out for the lunch deal if you are in Perth). For the first time in many years I wore a bikini in a public place! I had made it the day before using a pattern I’m trying out for a post surgical bra (the
Waves and Wild Superstar Bra, which is similar to the Evoe bra recommended by some ladies who've had reconstructions). I am now allowed to stop wearing the compression bra, but the surgeon said not to wear bras with underwires. I still need to wear the abdominal binder but I have been in firm, high shapewear for the last couple of weeks, rather than the thick elastic binder. I've made myself a binder from stable ponte fabric to wear at night. Anyway, back to the bikini. I hadn’t worn one for so long as I was self conscious about my tummy. Now I have my new surgically enhanced flat tummy (!) I am confident to wear a bikini in public. The lovely new breast is obviously very important too. It was an unexpected bonus to find this new confidence at all, let alone so soon after my massive surgery and all the associated stress.
So next for me is more waiting. This time for the Onchotype DX results, which take four weeks. I’m crossing everything it’s good news. UPDATE:
See the results here.